Op Note Documentation Tips Every Surgeon Can Use
You’ve submitted, in a timely manner, correct Current Procedural Terminology® (CPT) codes to the insurance company for the procedure you performed. The payor’s explanation of benefits (EOB) or electronic remittance advice (ERA) shows a payment of $0! Now what? Typically, you’d send in the operative note, showing the description of the procedure you performed.
The operative note is not only a medico-legal and patient care document. It’s usually the only information a payor wants when there is a dispute about your reimbursement.
So let’s walk through some key elements of the operative report documentation.
Pre-operative and Post-operative Diagnoses
All relevant pre- and post-operative diagnoses should be documented, including underlying co-morbid conditions that you consider relevant for the procedure performed. If a pre-op diagnosis is no longer relevant, or changes intra-operatively, then state this in the post-operative diagnosis statement.
For example, if the tumor or lesion pathology is not known pre-operatively, it is acceptable to state “unknown” in the pre-op diagnosis. If the frozen section comes back positive for a malignancy, this could be stated in the post-op diagnosis area.
Surgeon
The primary surgeon for the procedure is listed as the surgeon. In the academic environment, this is the attending surgeon for the procedure.
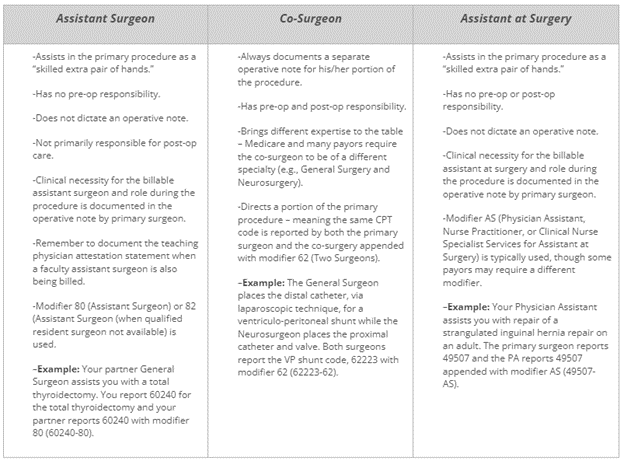
Assistant Surgeon vs. Co-Surgeon vs. Assistant at Surgery
Not crystal clear on the difference? Here are some tips that describe the different surgical roles typically seen in a procedure.
Procedure(s) Performed
The procedures performed are listed in this area of the operative note, which is typically on the top half of the first page. We recommend using CPT terminology as much as possible, but not including codes in the operative note. Why? Oftentimes, the codes documented in the operative note are not accurate.
It becomes a compliance issue when the codes in the operative report do not match the codes billed on the CMS 1500 claim form. Medicare’s General Principles of Medical Record Documentation state the CPT and ICD-10-CM codes reported on the health insurance claim form or billing statement should be supported by the documentation in the medical record. When a CPT code is documented in the operative report but not billed the CPT code billed is not “supported by the documentation in the medical record” as Medicare requires.
Indications for Surgery
This short paragraph, a couple of sentences, is very important as it provides the clinical necessity for the procedure being performed. It is also important to state any previous, related surgery on the same or different structure/wound, why patient is being brought back to the OR, or planned future surgery, as these are clues that coders use to support specific modifiers.
For example, a patient may require stages, of surgery to reconstruct an open wound which would warrant use of modifier 58 (Staged or Related Procedure or Service by the Same Physician or Other Qualified Health Care Professional During the Postoperative Period). Stating clearly that the staged procedures are prospectively planned, in this case, would tell the coder and payor that modifier 58 is warranted and the full allowable should be paid. All too often, when the planned nature of multiple procedures is not documented, a modifier 78 (Unplanned Return to the Operating/Procedure Room by the Same Physician or Other Qualified Health Care Professional Following Initial Procedure for a Related Procedure During the Postoperative Period) is used, which generally results in a payment reduction.
Complexity
This separate paragraph is a must if modifier 22 (Increased Procedural Services) will be used to obtain additional payment. This information should summarize the added complexity that will be in the subsequent details documented in the operative note. Don’t expect a payor to wade through the details of the operative note to try to figure out whether to pay you more. Make it easy for the payor to “feel your pain” of the procedure in a Complexity, or Findings at Surgery, paragraph.
Details or Description of Procedure
This is typically the lengthiest area of the operative note that describes the procedure(s) performed in great detail. Documentation should include, but not be limited to, induction of anesthesia, patient positioning, set-up and use of special equipment (e.g., stereotactic navigation, robot), specific brand name of any implant(s), which surgeon did what when more than one surgeon is involved, etc.
The details in this section of the operative note should support the procedures listed in the aforementioned Procedure(s) Performed area, which should also support the CPT code(s) reported for the procedure(s).